Editor’s note: In July of 2023 I published A Notre Dame Story that chronicled my son’s determination to get a Notre Dame degree , a process that coincided with some tumultuous events in my life, including a battle I had with cancer. That story is among the most widely read stories ever published by Fighting Irish Preview. What follows now is part 2 of that story: the details of my battle with cancer.
On Feb 26, 2022, my life took an unexpected detour. For about a month, I had been experiencing some low-grade sore throat symptoms and also I had noticed that my mouth seemed to be very dry, particularly in the morning. But otherwise, I felt fine and I didn’t really think much about it. Then on February 26th, I was driving home alone from Garver Lake in the South Bend area where I had visited my Mom and Dad. And I started thinking about my sore throat, that just wasn’t going away. I had an odd sensation that something was ‘stuck’ in the back of my throat. I started feeling around with my tongue in the back of my mouth and made a discovery.
I found a lump, about the size of a walnut in the back of my mouth near a tonsil. I opened wide looking into the rearview mirror, and I could see it.
Well, I thought, that’s not supposed to be there.
I was home in about an hour. It was Saturday afternoon and the plan was for me and Lynda to attend 5:00 PM Mass at our home Parish, St. Charles. It was about 4:30 PM and I said, “Lynda I have something I want you to look at.” Lynda looked and immediately said, “We are going to the walk-in clinic.” I did not argue.
I wasn’t scared at this point, but I certainly was interested in finding out what was going on.
We were able to get right in to see a physician’s assistant. One look and the PA knew this was not something routine. We talked a bit and she immediately made a referral.
Monday at 11 AM, I was sitting in the office of a specialist. “We will biopsy this”, the ENT doctor (who happened to be a Notre Dame graduate) said, “but I’m pretty sure this is cancer”.
Within a couple of days, it was confirmed. I had a form of cancer growing near one of my tonsils. The date was March 2, 2022. Lynda told me later that this news really hit her hard, which is not surprising, but my initial reaction was not quite like hers. My first thoughts were pretty matter-of-fact. Okay, this is part of the Lord’s plan. Let’s find out all we can about it, and make a plan to deal with it. The rest is up to God.
A CT scan within a few days held good news. The cancer did not seem to have spread, yet.
The next few weeks were a flurry of appointments, second opinions, and tests. Lynda and I spent a full day in mid-March at the IU Medical Center in Indianapolis. By this time the recommendation I had gotten in Fort Wayne was that I was not a candidate for surgery because of the placement of the tumor, but that a combination of chemotherapy and radiation should be sufficient to knock it out. This same course of treatment was also recommended by the excellent doctors at IU Med. Because it was our preference to not have to travel to Indianapolis for the treatments, we decided to go through treatment in Fort Wayne at the Parkview Cancer Institute.
At first, I was a bit relieved that I would not have to go under the knife for treatment of the cancer, and then I learned more about what I was facing. The prescribed course of treatment would entail 35 radiation treatments and 7 chemotherapy infusions over a span of 7 weeks. I was told that my prognosis was actually quite good, but that the treatments would be (in the words of our long-time family physician, Dr. Rich Kelty) “a bumpy road”.
That turned out to be an accurate description.
Overall what was happening to me, in my mind, did not seem particularly scary. My faith was strong. Certainly, there were moments of uncertainty, and Lynda and I shared some tearful moments. But I was accepting of my fate just as I was determined to fight this thing with everything I could muster.
One thing I then went about doing was informing the important people in my life about what was going on. Part of the reason I did this was with a selfish motivation. I wanted people to pray for me.
Most of those who I told, asked what they could do for me. My response was always the same, “Please pray for me.” I also handed out prayer cards with a favorite prayer, the Memorare printed on them to family and close friends.
Throughout my fight, those prayers and those people held me up. Visits, cards, gifts, text messages, and phone calls. My neighbor took over cutting the lawn, other neighbors helped with other tasks around the house and yard. Other friends actually sent over a landscaper to plant the flower boxes on our porch.
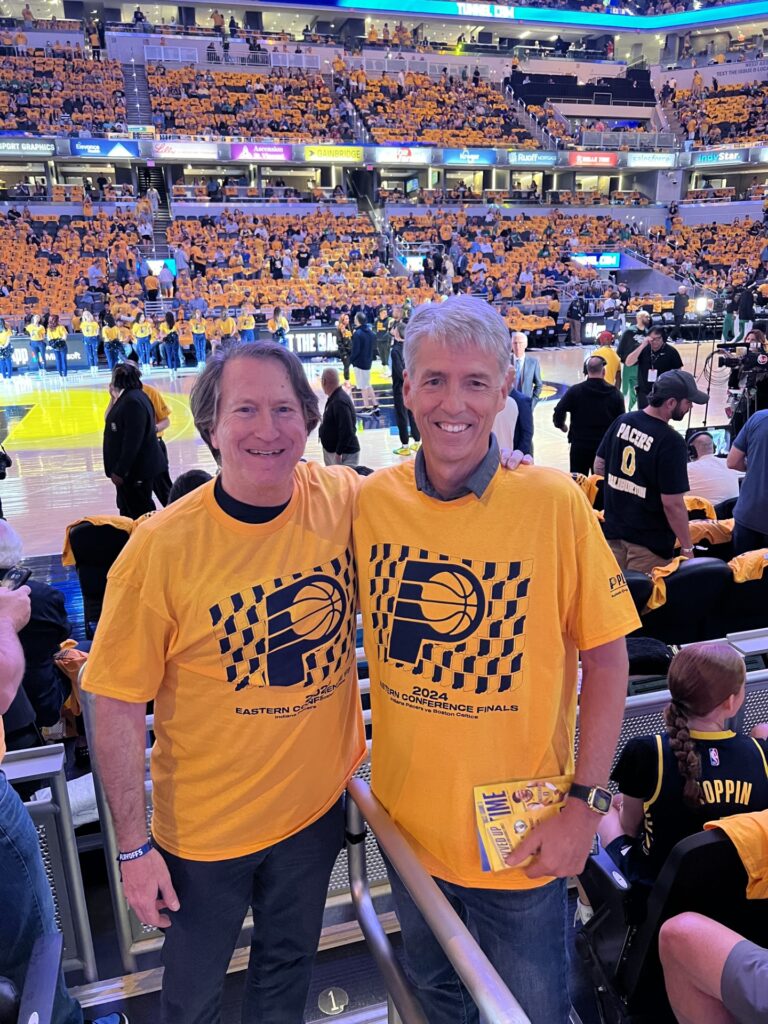
Me with long-time friend Art Mandelbaum at a Pacers playoff game in 2024. Art was one of those friends who really stepped up for me during the cancer fight.
Telling the kids was not easy. We got everyone together on a Facetime call and I matter of factly explained what was going on. The kids took the news quietly and with obvious concern. Soon however that concern changed to resolve that they would support me and Lynda above and beyond any call of duty. They did so.

Elsewhere, I have shared in detail the touching story of how I told my elderly Mom and Dad the news, and their reaction. They offered their prayers, hugs and encouragement throughout, and said a daily Rosary for me.
Those prayers that were offered for me, lifted me. They sustained me. They comforted me and they strengthened me. I was driven to do everything I could to get better and to have a positive attitude as “we” fought. And I use the word “we” on purpose. Throughout I felt the positive energy of all those prayers lifting me.
Fighting my cancer was also a “we” effort between me and Lynda. Of course, there were many friends, Doctors, other medical personnel and the rest of my family that played roles. But Lynda’s role was, BY FAR the biggest, and for the most part thankless. Fortunately, we were in a situation financially where Lynda was able to retire from her job heading up the Vera Bradley Breast Cancer Foundation so she could work for me, full time. The situation with Lynda’s “retirement” was made possible by Vera Bradley corporate being fair and understanding of our circumstances.
Because of her “retirement”, Lynda was able to be at every appointment I had (and there were a lot of them), she kept track of where I needed to be and when. She made sure all the prescriptions I was on were filled, and that the meds were taken by me at the right time. She prayed with me, laughed and cried with me, encouraged me, and fed me (literally!). Simply put, she loved me.

People marveled at the positive attitude I maintained throughout, it was only possible because of Lynda. I focused on getting well, and Lynda did everything else. I know all this was exceptionally tough on Lynda. She has since shared with me her many moments of loneliness, feelings of stress, and anxiety. Despite all that, she was unflappable in her support of me.
The issue of my own career as a Magistrate with the Allen Superior Court and how my caseload would be managed during my reduced capacity to work was a major issue. Fortunately, my colleagues on the Court made it clear to me early on that they would support me 100%. When all was said and done, I was off of work for three months. I think that the fact that I had taken only two and a half days of sick time in 37 years on the job may have played into the support I received from the Court, but I can’t express my gratitude any stronger for what the Judges did to support me. I particularly am indebted to Judges Craig Bobay, Jennifer DeGroote and Tom Felts. My long-time court reporter, Kim Kendall, also stepped up in a big way, beyond the call of duty, to keep my court running. This took an enormous burden off my shoulders.
Another thing I did shortly after the diagnosis was to call Father Tom Shoemaker, the Pastor at our Parish, St. Charles Borromeo. Lynda and I had joined St. Charles when we moved to Fort Wayne in 1986, and it has been our spiritual home since, it is located very near our house and all three kids graduated from grade school there.
I made an appointment to see Father Tom later that day, after work. I don’t remember a lot about our meeting but it was very emotional. I told Father Tom about the cancer and I made a “General Confession”. A general confession is where you confess to a Priest not just the sins you have committed since your last confession, but ALL the sins of your life. I was aware of the concept and I knew that it was a recommended practice at times of major life transitions.
Well, I had cancer and this was the time.
That’s right, all my sins, my whole life. My confession lasted about 30 minutes and Father Tom was wonderful. The amazing grace of the sacrament of Penance was received and I walked out of Father’s rectory office feeling a profound sense of peace and resolve.
I was fortified spiritually for the fight I was about to face.
One of the toughest times I experienced during my fight was during the period between diagnosis and the start of treatments. My first day of treatment was scheduled for April 12, 2022, just about six weeks after I was diagnosed. During this time period, my throat was getting sorer almost by the hour and I knew the cancer was growing. I wanted to start fighting back! But a lot of necessary preparations and tests had to be completed before the actual treatment could start.
One day I was at the Cancer Institute at Parkview Hospital in Fort Wayne to go through another test and consultation to get ready for the radiation treatments. Something required a nurse to give me an IV. I’m not a big fan of needles, but I’ve always tolerated them okay. This time was different, and it turned into a crazy adventure!
The nurse for some reason had a difficult time finding a vein and she had to poke my arm several times. On her third or 4th try, the long day I had already had and the growing cancer in my mouth got the best of me. I blacked out, slumped over, fainted.
It took a few moments but the nurse and Lynda got me back to consciousness. A minute later though, it happened again. I have a vague recollection of the nurse’s reaction as I was going out the second time. You know how on those TV medical dramas when an emergency occurs in a hospital they hit a button, an alarm sounds and people come running? Well, that is what happened to me!
The next thing I knew I was lying on a gurney a few feet from where I had fainted and the cavalry, had arrived! About a dozen people were standing around me and out into the hallway. I was hooked up to a vital signs monitor. I noticed that my blood pressure was super low, like 50 over 30, but it was starting to climb. Let me tell you if you are going to faint, do it in the hospital! Working on me were two Doctors. I don’t know who they were but they could have been starring in one of those TV medical dramas! Young and handsome and in charge! Other nurses and various staff were also in sight, I saw the hospital chaplain, who I had already gotten to know over in the corner, she was standing with Lynda.
The Doctors were great and within a few minutes my vital signs returned to normal and I was feeling much better. Nonetheless, I was ordered to move to the emergency room.
The emergency room at Parkview North is connected to the Cancer Center, by a long walkway. In total, it was about 300 yards from where I was laying.
Despite the close proximity, the protocol was that I had to be transported… by ambulance! In walked three EMS guys, dressed in spiffy flight suits. The crew that came for me happened to be the one that typically handled the helicopter “Samaritan” flights. This crew “responded” because they are based right in the hospital. I noticed they had nicknames embroidered on their suits something like “Cougar” “Ace” and “Skywalker”.
From this, I figured I had a pretty good crew.
The Doctors turned me over to the EMS crew and I was soon transported outside into a waiting ambulance. I was feeling fine by this time so I just decided to go with it all. I think I asked if I could turn on the siren, lol. Once I was in the ambulance I heard the radio call to the emergency room, “ETA 30 seconds”. Really!
So I went on the world’s shortest ambulance ride, about 100 yards! In the emergency room I was given all kinds of tests and nothing irregular was found. After a couple of hours, I was sent home.
The procedure I had missed due to my fainting adventure was rescheduled for a couple of days later. This was the appointment at which a mesh mask was molded for me for the purpose of securing my head and shoulders in the tunnel during radiation treatments. This also turned into an adventure and not a very fun one.
Head and neck radiation requires the creation of a mesh “mask” which closely fits over your head and shoulders and can be locked down to the radiation table (The photo at the top of this article shows me with the mask on). This is necessary because, for precise targeting purposes, the head and neck must be kept as still as possible. The process of creating this device required me to first lay on an actual radiation table, a frame was then placed over my head and shoulders and “locked” down to the table. Warm, pliable strips of some kind of plastic are then laid in a latticework fashion over the face and the frame. There is then a wait time of about 30-40 minutes while the mask cooled and hardened into a custom shape of my head and shoulders. During the wait time, my job was to lay as still as possible in the dimly lit radiation room.
Sounds pretty easy, but it wasn’t for me.
The tech set this all up, checked if I was okay, and then left the room. At first, the warm mask strips felt good on my face, but pretty soon the sensation of my eyes, ears and mouth mostly covered by this mesh and my head being locked down caused me to experience claustrophobic anxiety. This was awful and I had no idea of how much time was passing and I really couldn’t remember how long I was going to be laying there. Typically, I can handle moments of anxiety pretty well. Mostly I just close my eyes and pray. That is what I did but with blurred vision from the mesh, extra heat from the molding process, and a feeling of loss of control, I didn’t do well. I battled the anxiety with every trick I could think of but I wanted to scream. I didn’t, but I came close. I was miserable and felt like I never had felt before. Fortunately, I got through this but immediately thereafter, I realized that over the coming weeks, I was going to be receiving 35 treatments that were going to require me to be locked down on that table under that mask.
My feelings about that continued to cause anxiety.
The night after this experience I had a terrifying nightmare and started screaming and thrashing around in my sleep. Lynda eventually got me awake and back to some sense of reality, but I was not in a good place. At this point, through tears, I confessed to Lynda the anxiety I was having. At about three o’clock in the morning, Lynda and I talked it through and she got me calmed down. We prayed together and I got through the night.
The next day I fortunately, after a little research, discovered that my reaction to “the mask” was not uncommon. I discovered some ideas to help me with the experience. The first was medication. I found that some patients actually had to be heavily sedated to go through the process. I also read that if a few small eye holes were cut in the mask it would reduce my sense of claustrophobia. On my own, I came up with the idea that if I could listen to music during the process it would help me a lot.
We had an appointment with the palliative care doctor a few days before the treatments were to start. I thought this appointment would present a good opportunity to discuss my anxiety over the upcoming radiation treatments. At the appointment, the Doctor, who we were meeting for the second time, was very compassionate toward my concerns, and her verbal encouragement bolstered me. She did not think I needed “heavy sedation” but she did prescribe a mild sedative to be taken before the radiation sessions. She actually told me she thought I would do just fine, she pointed out that the actual radiation sessions would be much shorter than the preparatory session I had been through and that also made me feel better.
We also learned that it would be okay to bring my own music to listen to during the treatment and that cutting holes in my “mask” would be discussed with the radiation techs before my first treatment. This was an example of the way things were communicated between offices efficiently at the cancer center.
I had been assigned a “team” that included a radiation Doctor, chemo Doctor, a palliative care Doctor, a dietician, a speech/ swallow therapist, a social worker, a Chaplin , and another team to look after my feeding tube, that would become necessary during the course of treatments. The whole team was tied together by a nurse concierge who was also assigned. Any question that came up at any time, we would know who to call. If we weren’t sure, we contacted the concierge and they were wonderfully responsive.
A few days after the palliative care appointment, the time had finally arrived. It was time to start fighting back against the cancer. The date of my first treatment was April 12, 2022, a Tuesday. For the next seven weeks, I was to undergo five radiation treatments a week, Monday through Friday, and seven chemotherapy treatments each Tuesday. If all went to schedule, my last day of treatment would be May 31st.
April 12th arrived. Chemo took place each week early in the morning, generally at about 7:30 AM, and would last for about 5 hours. The radiation treatments were every day at 10:30 AM, except on chemo day when they took place in the afternoon.
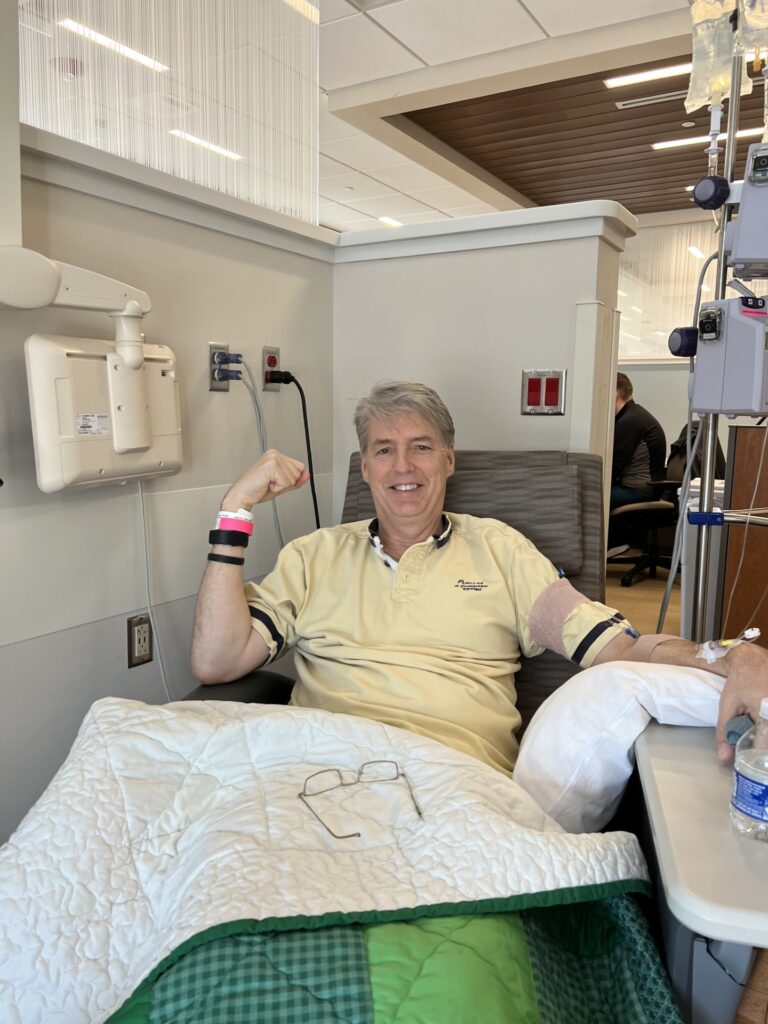
We started on a Tuesday so the first day of treatment would include both. The first step was to get blood count levels. As soon as the lab results came back (usually in about 30 minutes), the results went to the chemo Doctor who would then customize the chemo drug to be administered. I would recline in a comfortable chair in a semi-private cubicle and the nurses took over. For the first treatment, AJ was in town to provide support, which was greatly appreciated by both Lynda and I. He was present in the room along with Lynda. The nurses were great. They carefully explained every step of the process that started with establishing an IV and then flowing in various things from saline to keep me hydrated to antihistamines and steroids to counteract the chemo side effects and also of course, in flowed the chemo drug.
The side effects and pros and cons of the chemo had been thoroughly discussed with us in an earlier appointment. Among other things, I was told that I would not lose my hair from this particular drug, but that I might encounter ringing in my ears that could lead to permanent hearing loss. That of course got my attention, I was happy I would not lose my hair of course, but I had to be careful to report any ringing in my ears during the seven weeks.
The first chemo went well, I rather enjoyed all the attention. The Chaplin came in to talk and to pray with me, the social worker spent time with me and the nurses really made a fuss over me. Lynda and I were able to order “room service” from the hospital cafeteria. This became the routine for all the following chemo treatments, although they didn’t all go 100% smoothly!
After the first chemo treatment, I moved downstairs from the cancer center to the radiation area. I was feeling better about the radiation and took the mild sedative that had been prescribed, but the anxiety was not gone. I first met with one of my techs and explained what I had been feeling. She was great, she said they welcomed my music (I had my phone and a Bluetooth speaker) and she cut eye holes in my mask.
The first radiation went smoothly. The music was fun (each day I created a new three or four song playlist), eyeholes helped, and the whole process lasted about 12 minutes. My first day was in the books.
6 more chemo’s and 34 radiations to go.
In the coming weeks, Lynda and I fell into a routine. Except for Tuesdays when the day started earlier because I had chemo, we would leave for the Cancer Center at about 10:05 each day. On the way, she and I would say the Rosary together. The timing seemed to work perfectly, it was a 15-minute trip and that is just about exactly how long it took us to say the Rosary. After treatments were over, we would head home and generally speaking I would head straight for the couch in the den. Particularly as the number of treatments accumulated I felt more and more sapped of strength and just flat out tired.
Over the coming weeks during my daily couch sessions, I learned just about every detail of the TV channel schedules, watched dozens of documentaries, and a lot of Cubs baseball. I think I have now mastered the subjects of WW II, the Civil War and the life of every classic rock artist of any significance. I also think I saw every episode of Pawn Stars and American Pickers, and those shows have been on the air for a LONG time!
A couple of weeks into the treatments, I went through a minor surgical procedure and had a feeding tube installed. Those who undergo the type of treatments I underwent, almost without exception, start to lose interest in and the ability to eat, and they lose weight. We had been told that this would occur in advance and it did, so having a feeding tube was a necessity. Sure enough, by the 4th week, tube feeding was becoming a necessity, because it was about all I could manage to just drink some water. Even high-calorie drinks like Ensure and Boost became tough to swallow. I lost about 20 pounds, but once we went to full tube feeding, my weight stabilized.
One thing that was on the horizon from the start of all this was the impending graduation of Nick from the Masters of Accountancy program at Notre Dame. My love of Notre Dame and Nick’s “Notre Dame Story” had me determined to be present for all the graduation festivities which would take place the weekend after I had gone through five weeks of treatments. I had one person tell me that the only way it would be possible for me to be there would be if I was in a wheelchair.
I was determined to be on my own two feet for the events. I made it, but just barely!
While the radiation was doing a slow but surely accumulating amount of damage to my mouth and throat, each week chemo had me riding an energy roller coaster. This was because of the large doses of steroids that were administered with the treatments. I actually would come out of the treatments and feel pretty good energy-wise for a couple of days. The steroids were administered during the treatments and then supplemented for the next three days. Then starting Saturday, I was off them and I could feel myself start to decompensate. Lethargy took over and by the end of the weekend, there wasn’t much else I wanted to do but sleep. Then by Tuesday, I was wiped out, barely able to walk, but with the next treatment, the process would start again.
After the second chemo treatment, I reported that I was experiencing some ringing in my ears. Because I had been warned of this possibility and its possible implications I immediately reported it to the chemo Doctor, Rob Manges. The chemo drugs I was getting were changed to counteract this and the ringing did stop. But, I was told that with the new chemo drug, I would lose my hair. When I heard this I cried. I knew my hair would grow back, but this really affected me. One of my first calls upon learning this was to Mike Ehle, who had cut my hair for over 30 years. Mike did not hesitate when I asked if he would make a house call and give me a really short, “chemo cut”. That done, a few days later a package arrived and Lynda got all three kids together on a Facetime call so that I could open it up. Inside were three really nice hats-Notre Dame, Cubs and one I’ll describe as “chic dri fit”, for me to wear as I lost my hair.
To make a long story short, despite the new chemo drug, I never did lose my hair. I am told that avoiding that was rare. Thank God! And I got some really nice hats from my kids out of the deal!
So, Nick’s graduation weekend of May 14-15 arrived and mentally I was determined to experience his Notre Dame graduation to the fullest. Physically I was not doing so well, but I wasn’t in a wheelchair as I had been told to expect. At least not yet.
The festivities started with the Baccalaureate Mass which was held in Purcell Pavilion on Saturday evening. It was a beautiful ceremony and I think just about every important person on this side of the Pope was present to honor the graduates. Fortunately, it involved a lot of sitting and I tolerated it well. We had dinner back at the townhouse Nick lived in with four other students in his program and then headed over to my niece Sara’s house in South Bend where we spent the night. Sara is a nurse, and having her close at hand was reassuring.
Up at Garver, my Dad who was just a few days short of his 98th birthday had really taken a turn for the worse. He had been in Hospice for a month or two and was now bedridden. Throughout the weekend, I spent some time at his bedside holding his hand and talking to him and praying. He was awake but was not able to clearly speak. We showed him photos we had taken of Nick in his graduation sash standing in front of the Golden Dome, he weakly but most assuredly, smiled.
We knew that my Dad’s time on earth was short.
On Sunday morning we were up early on a beautiful Spring day and headed to ND Stadium for the school-wide graduation ceremony. The Notre Dame campus was in its glory. I had to take my time but I managed to get myself from the parking lot to seats in the stadium without much assistance. I did however have my family all around, watching me like a hawk.
The graduation ceremony was long but impressive. We were able to pick Nick out as he processed in and he found us up in the stands. That was a sweet moment. After the Stadium graduation, we moved to the area between the stadium and the Library where many of the graduates gathered for pictures and celebration. By this time I was getting worn down. It was a long day and the chemo/steroids from the previous Tuesday were definitely wearing off. But I soldiered on, posed for the pictures and joined in the celebration.

We then went back to Nick’s townhouse for a planned party. Nick’s roommates also had family there and I remember how kind they all were to me. After a few minutes at the party, I excused myself and went to Nick’s bedroom to lay down. I was wiped out and the general soreness in my mouth was causing a pounding headache. I laid down for a couple of hours and that helped. One more event to go.
The next event started in the late afternoon and was the diploma ceremony for the accounting graduates. This event was wonderful. Two professors addressed the relatively small gathering of graduates and families. They were funny and inspiring, I remember that. I also remember feeling miserable. My head was pounding and I just was feeling generally uncomfortable. During the ceremony, it was announced that Nick was the recipient of the prestigious Brother Cyprian award for his academic achievement. A proud moment indeed. After receiving his diploma, Nick walked right past where we were sitting after leaving the stage. He stopped and gave me a hug, and tears welled through my misery. Something about what I was going through intensified the significance of such moments, and graduations of course are big moments.
Afterwards, there was a reception for all the students and families in a nearby building. I made it to the reception and found the first chair I could and sat. I was not well. We stayed only a short time. I felt a bit guilty about the quick exit but I needed to leave. We made it up to Garver for another party for Nick, I headed to the guest room and laid down. I really don’t remember much from this gathering.
After a couple of hours, we headed back to my niece’s house to call it a night but not before saying goodbye to my Dad. He seemed to be comfortable but was unable to communicate. I held his hand, prayed, and told him what I could about Nick’s graduation. I was pretty sure it would be the last time I saw him.
Once back at Sara’s house, it was nice to have a nurse in Sara to help Lynda in making me as comfortable as possible. Soon I went to bed for the night, coughing fits, and a pounding headache notwithstanding.
I had made it through the graduation ceremonies, but just barely.

The next morning we headed back to Fort Wayne and straight to a radiation appointment. I was the weakest I had ever been but I got through the appointment.
That night was awful, headache, coughing, fatigue, and now I was running a temperature. Up until that point I had resisted taking the opioid-based medicine that had been prescribed for me, but I gave in and asked Lynda to give me a dose.
It had to be administered through the feeding tube.
Then we got the call from Garver, my Dad had passed away. Not unexpected, but it still hit hard. Now I had a funeral and the responsibility to pay proper tribute to Dad on my mind.
On Tuesday morning, we headed to Parkview for chemo, but after the lab results came in from my blood work, the Doctor canceled the appointment. My white blood cell (the cells in charge of fighting off infections) count was too low. My body was in such a weakened state that it would not be safe to do the chemotherapy. Previously, we had been advised that if my body temperature exceeded 102 it would not be safe to do a radiation treatment.
Already emotional from the loss of my dad, this really hit me hard. I had been so focused on getting through the treatment schedule that any deviation was a significant blow. I remember lying on the couch a few hours later and working on a reset of my internal sense of resolve. How you deal with adversity was something I had always talked to my kids about. You can do one of two things, deal with it, or fall to pieces.
Prayer got me through and I dealt with it.
Later that afternoon we were still scheduled for a radiation treatment, I did not want to miss it and I asked Lynda not to tell the radiation techs about my elevated body temperature, until after the treatment. She of course ignored this request and upon arrival, announced that I had a temperature. The temperature was confirmed and they canceled my appointment. A few minutes later after I was examined by a Doctor, and I was sent to the emergency room. I was weak, I was uncomfortable, and my ability to fight anything off due to the low white blood cell count was almost nonexistent.
After a bunch of tests and x-rays, I was admitted to the hospital, apparently with pneumonia.
Hospital life was something I had never experienced. Early on during my stay, I realized that it was going to be difficult to live up to my responsibilities to honor my dad and to plan a funeral. Fortunately, despite my reduced capacity, I was able to help some and everyone else stepped up and took care of the rest.
My sister Peggy, did a wonderful job of taking care of funeral details. It was set for Saturday morning in South Bend, and our longtime family friend, Monsignor Bill Schooler agreed to perform the Mass. “Father Bill” had been the Chaplin at Marian High School when I attended there from 1975-1979. He is a Priest’s priest. I love and respect him very much.
In the meantime, I had to focus on doing what I could, while laying in a hospital bed. I wrote an obituary and eulogy lying there while packed in ice to get my body temperature down. Fortunately, AJ, who had been in town for the graduation had had his flight delayed and then he cancelled it and stayed in town to help out.
Oh, did I mention that the day after I landed in the hospital, it was Lynda’s landmark, 60th birthday? It was, and we celebrated it in the hospital room. AJ brought balloons and I had a few gifts that I had bought in advance. Not exactly a party for the record books, but we did what we could. God Bless Lynda.
While in the hospital I fell into a good rhythm of consistent and regular tube feeding, treatments to ease the pain in my mouth and got lots of rest. After a day or so, my temperature started coming down and I was feeling better. The doctor said he would not release me until I had a normal temp for 24 straight hours.
By Thursday night it was pretty obvious that I would miss my Dad’s funeral. Wow. AJ agreed to deliver the eulogy I had written. That made me feel better because AJ was perfect for delivering it. Lynda arranged to have my friend Lantz Mintch stay with me during the funeral, which would be live streamed so I could watch on my laptop. I hated that I couldn’t go, but admittedly I knew that in my condition it would have been a struggle, not to mention against Doctor’s orders.
By Saturday morning I was feeling even better, my white blood cell count was improving and the temperature was back close to normal. The funeral was at 9 AM and was beautiful, Father Bill was great. I was gratified to see so many friends of mine, in attendance.
Timing issues caused us to schedule things a bit out of order and my Dad’s “wake” was held at the Church after the service. During this two-hour time frame Lynda carried around her phone and I “Facetimed” with many friends and relatives who were in attendance. Eventually, she moved up to the casket and I got to spend some time with my Dad. I cried like a baby, but got to say my goodbye. I know my dad understood my absence.
AJ delivered the eulogy in superb fashion. The ceremony then moved on to the cemetery which I also got to watch. As a decorated WW II vet, my Dad got a full military send-off. It was as beautiful as it was deserving.
And the funeral was over.
On Sunday, after 4 nights and 5 days, at last, I was released from the hospital. I was still weak. I could only walk short distances and my sense of balance was compromised. The radiation had left my face and neck skin red and peeling. I was down 20 pounds, facial hair, nose hair and a strip of hair on the back of my head was gone with no sign of returning.
The good news at this point was that the periodic scans I had been getting showed that significant progress had been made in eliminating the cancer.
It was May 22, 2022, almost three months since I had been diagnosed with cancer. I had 7 more radiation treatments and two more chemos to go.
On May 31, I underwent chemo number 6 without incident. The only problem was the fact that the veins in my arms had basically turned to “spaghetti” (a term applied to a common condition among chemo patients) and it was really difficult to put an IV into my arm so the drugs could be infused. The process was excruciating as I recall, multiple “sticks” and quite a bit of “fishing” for a vein.
My chemo doctor on that day informed us that because I had missed one chemo while hospitalized and the scans were all looking good, it would not be necessary to undergo the seventh treatment as it would have to occur after my radiation was complete. I had a strange reaction to this suggestion. My reply was this, “Doctor, I signed up for SEVEN, the mission I have focused on for the last three months included SEVEN, unless you tell me it would be counterproductive or otherwise harm me, I want #7.”
The Doc scheduled me for #7.
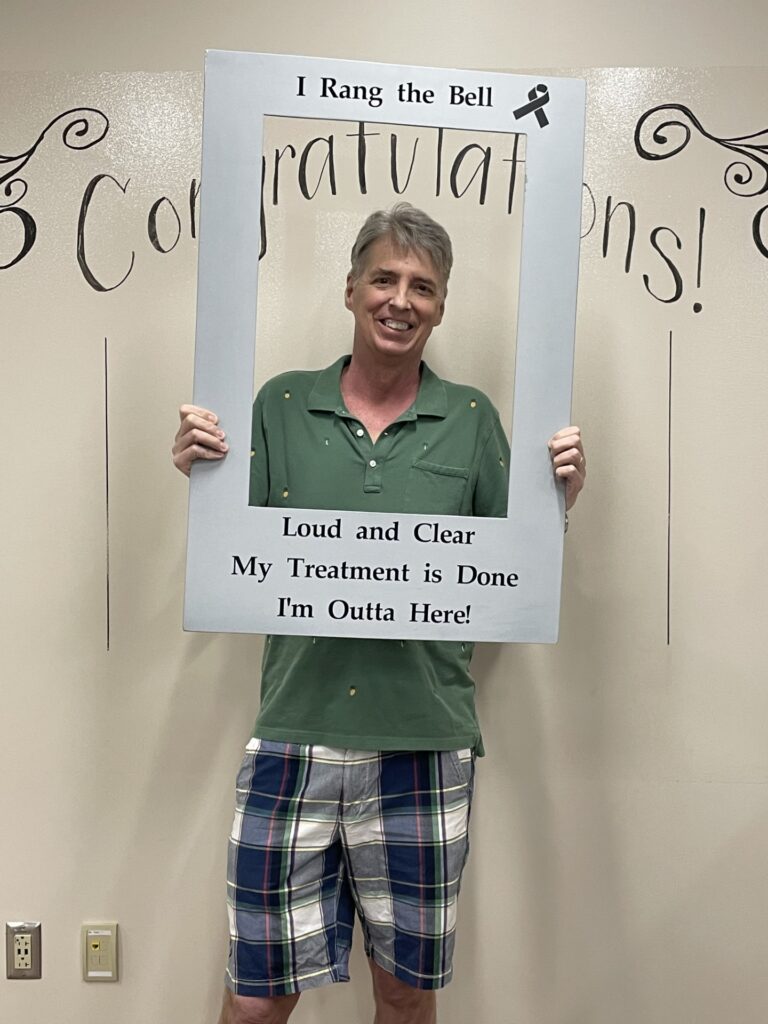
On June 1, I had my 35th and last radiation treatment. It was a moment of celebration. I “rang the bell” after the last treatment. It was a bittersweet moment because I also said goodbye to the techs and other compassionate staff and volunteers. They had been wonderful for what they had done for me and how they had treated me. Several presented me with cards that expressed beautiful sentiments. We even got a card from one of the other patients who was undergoing treatment for prostate cancer and had daily appointments at the same time as me. These people had all observed my cancer journey with a front-row seat, and I grew to appreciate them and care about them a lot.
On June 3, 2023, I had my last chemo treatment. Again, I had a lot of wonderful people to say goodbye to that day.
I went home that day and as usual, headed for the couch. I was a mess physically. Fatigued, on 100% tube feeding, unable to open my mouth without pain, mouth sores, peeling skin, general aches, constant coughing, it hurt to talk and my voice was weak and more. But the mission was accomplished, 35 radiations and 7 chemos.
Now it was time for my recovery from the treatments to begin.
Speech and physical therapy, slow weaning off several drugs, the reintroduction of actual food and exercise into my life and many more “check-ups” with my doctors, ensued.
The recovery period to this day goes on.
As this is written I am 24 months past my last treatment. All the scans I have had since show no evidence of cancer. I still have latent “reminders” of my journey. My mouth is still a bit “raw”, and I have trouble producing saliva, but I’m alive and living a great life.
Let there be no doubt that cancer is a monsterous foe but it is not insurmountable. Most profoundly however I feel that my cancer fight journey served as a validation of my faith.
I will always be thankful to Lynda, my other family, friends, doctors and staff, and to God for getting me to where I am today, healthy and proud to be a cancer survivor.


